https://www.texastribune.org/2021/05/10/texas-governor-emergency-powers-pandemic-legislature/
Author Archives: Unlocked
“There is not a single documented Covid infection anywhere in the world from casual outdoor interactions, such as walking past someone on a street or eating at a nearby table,” the NYT reported.
SC/MT ENDING THE VIRUS PANIC HOAX PAY
The states of South Carolina and Montana have both decided in recent days to put an end to their handouts of federal unemployment benefits as a result of the coronavirus pandemic, in an effort to encourage residents to return to the workforce, as per CNN.
Montana Governor Greg Gianforte (R-Mont.) said in his announcement that “incentives matter, and the vast expansion of federal unemployment benefits is now doing more harm than good. We need to incentivize Montanans to return to the workforce.” Instead, Governor Gianforte announced that the state government will be providing $1,200 checks as bonuses to every citizen who returns to work, using the state’s share of the recent $1.9 trillion stimulus package to pay for it.
In South Carolina, Governor Henry McMaster (R-S.C.) announced on Thursday that the state would be ending their share of federal unemployment benefits, since “what was intended to be a short-term financial assistance for the vulnerable and displaced during the height of the pandemic has turned into a dangerous federal entitlement, incentivizing and paying workers to stay at home rather than encouraging them to return to the workplace.”
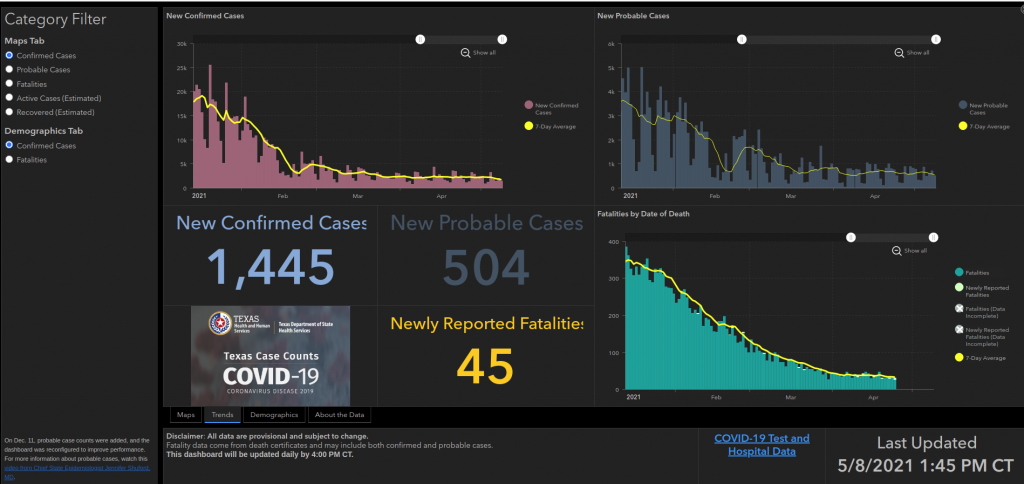
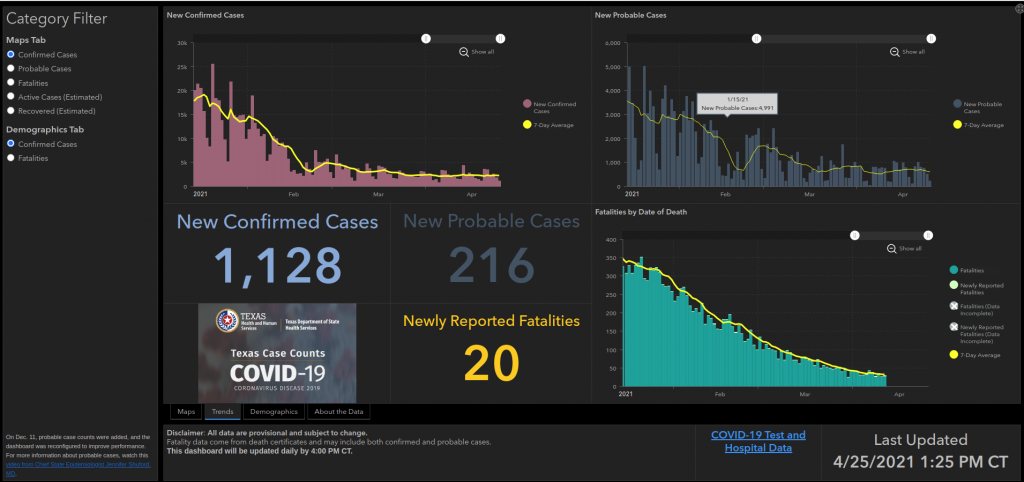
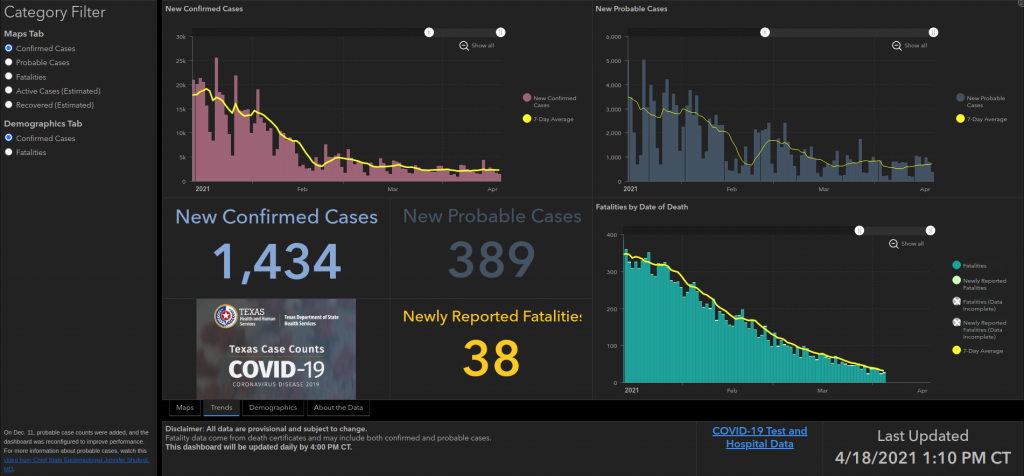
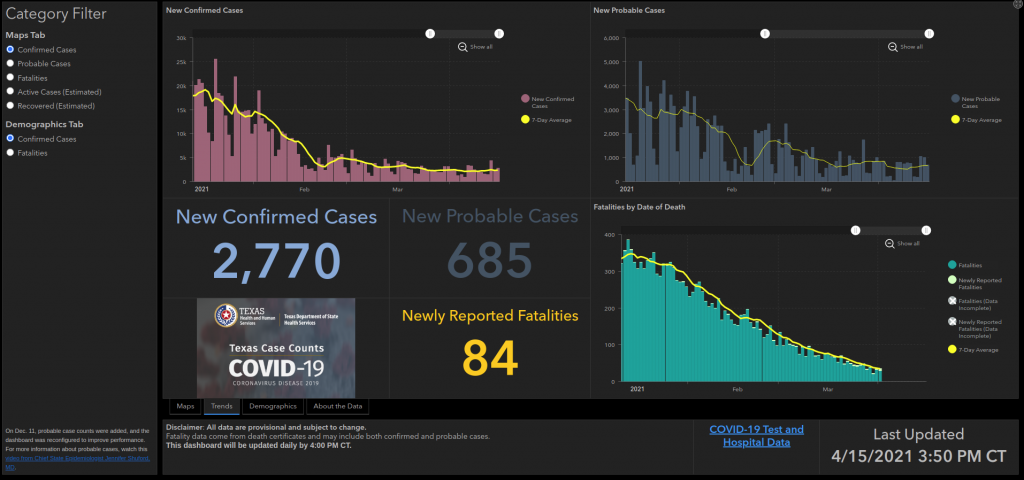
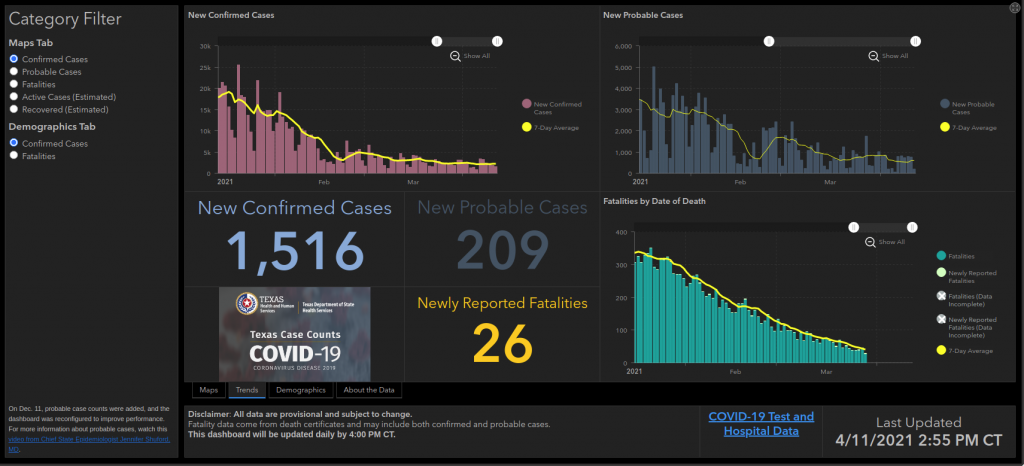
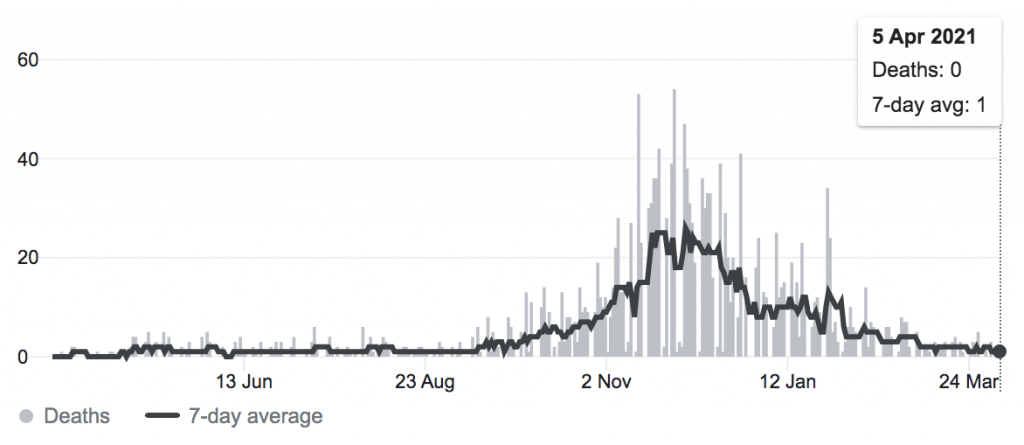
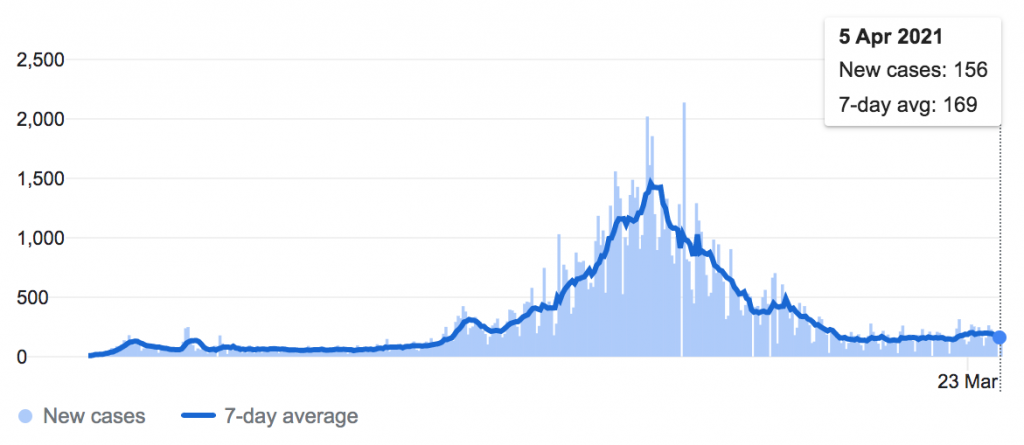
Casedemic still declining in TX after face diaper distancing hoax mandate dropped
–NIH RETRACTED FACTUAL STUDY OF FACEMASKS BEING WORTHLESS
- WE SAVED THE ARTICLE ON NO-LOCKDOWN.COM
- https://www.no-lockdown.com/index.php/2021/04/18/5627/
- LINK TO ORIGINAL ARTICLE SAVED, ABOVE
Med Hypotheses. 2021 Jan; 146: 110411.Published online 2020 Nov 22. doi: 10.1016/j.mehy.2020.110411PMCID: PMC7680614PMID: 33303303
RETRACTED: Facemasks in the COVID-19 era: A health hypothesis
Baruch Vainshelboim∗Author informationArticle notesCopyright and License informationDisclaimer
Abstract
This article has been retracted: please see Elsevier Policy on Article Withdrawal (https://www.elsevier.com/about/our-business/policies/article-withdrawal).
This article has been retracted at the request of the Editor-in-Chief.
Medical Hypotheses serves as a forum for innovative and often disruptive ideas in medicine and related biomedical sciences. However, our strict editorial policy is that we do not publish misleading or inaccurate citations to advance any hypotheses.
The Editorial Committee concluded that the author’s hypothesis is misleading on the following basis:
1. A broader review of existing scientific evidence clearly shows that approved masks with correct certification, and worn in compliance with guidelines, are an effective prevention of COVID-19 transmission.
2. The manuscript misquotes and selectively cites published papers. References #16, 17, 25 and 26 are all misquoted.
3. Table 1. Physiological and Psychological Effects of Wearing Facemask and Their Potential Health Consequences, generated by the author. All data in the table is unverified, and there are several speculative statements.
4. The author submitted that he is currently affiliated to Stanford University, and VA Palo Alto Health Care System. However, both institutions have confirmed that Dr Vainshelboim ended his connection with them in 2016.
A subsequent internal investigation by the Editor-in-Chief and the Publisher have determined that this article was externally peer reviewed but not with our customary standards of rigor prior to publication. The journal has re-designed its editorial and review workflow to ensure that this will not happen again in future.
The Editor-in-Chief and the Publisher would like to apologize to the readers of The Journal for difficulties this issue has caused.
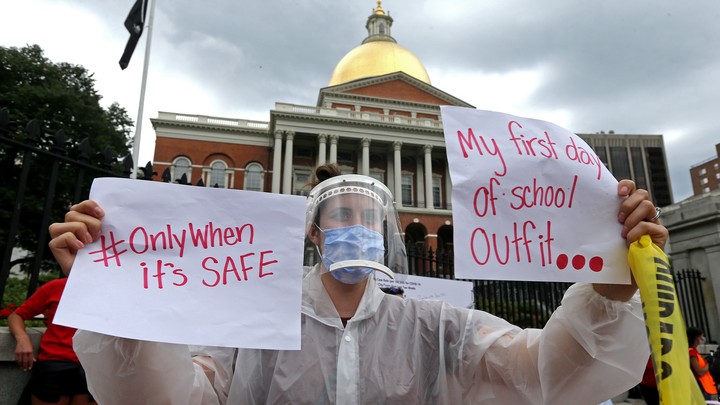
“teachers” with Mental illness
- these people are “teaching” your children !
Centers for Disease Control and Prevention (CDC) Director Rochelle Walensky defended masking requirements for children in outdoor summer camps on Wednesday, arguing situations surrounding sporting events could be dangerous.
FED COURT says CDC cant stop evictions.
https://m.theepochtimes.com/federal-judge-sides-with-landlords-vacates-cdcs-eviction-moratorium_3803808.html/amp
Stop obeying!
Masking
Distancing
Stay home
The peer-reviewed study, published in the scientific journal PNAS, found stay-at-home orders (also known as shelter-in-place orders or SIPs) were not associated with lower infections or deaths; furthermore, they were actually associated with a slight increase in infections and deaths, although this was not statistically significant
It’s never going to END America. Unless you refuse to comply.
If only it was a joke

STOP OBEYING!
- Everyone at the camp—including staff and every kid over the age of two—must wear masks at all times, unless they are eating or swimming. They should wear two layers of masks, especially when social distancing is difficult, regardless of “whether activities are indoors or outdoors.”
- Campers should be placed in “cohorts,” and their interaction with people outside the cohort must be limited.
- There should always be at least three feet between campers of the same cohort, and six feet between campers of different cohorts. Staff should keep six feet away from campers at all times, whether inside or outside. Distance should be maintained while eating, napping, or riding the bus: The CDC suggests seating kids in alternating rows.
- The use of physical objects that might be shared among kids—toys, art supplies, electronics—should be limited wherever possible.
- Camps should not permit close-contact sports and indoor sports, and should require masks regardless.
- If anyone is curious there are separate restrictions for outdoor gardening.
MURDERERS!
- STATE GOVERNORS WHO MURDERED THEIR OWN PEOPLE

data, collected from 113 hospitals who surveyed patients over a three-day span, suggested more than two-thirds had contracted the virus while staying at home.
WORST GRAMMA KILLER .GOV IN THE NATION HAS ADVICE HOW TO NOT KILL GRANNY
-CDC SHOULD BE DISREGARDED-
- MASKING = HOAX
- DISTANCING = HOAX
- CASEDEMIC = HOAX
Cotton said, “The CDC is a thoroughly politicized agency. Most Americans disregard their advice on things like steaks and hamburgers and beers. Increasingly, they should disregard their advice when it comes to school reopenings. Schools need to be open. Schools have been open in Arkansas five days a week, in-person since last August, and it’s been largely fine. That’s been the case all across the country as well. We shouldn’t have a politicized public health bureaucracy like the CDC answering at the beck and call of the teachers’ unions. We need kids back in school, and back in real school, not sitting in a classroom doing a Zoom session with teachers who are not in the classroom. We need kids in schools with their teachers now.”
FL ENDS THE PANIC HOAX!
May 3 (UPI) — Florida Gov. Ron DeSantis on Monday signed an executive order dropping all local emergency COVID-19 pandemic restrictions across the state, citing progress in vaccination efforts.
The debate is over.
https://nypost.com/2021/05/01/covid-lockdowns-cost-jobs-dont-appear-to-have-saved-lives/
Tyranny on full display
Michigan Gov. Gretchen Whitmer (D) said Thursday she will ease coronavirus restrictions on the state when enough residents submit to receiving a vaccine.
The astonishing level of mental illness exhibited by democrats
Joy Reid “I am among the fully vaccinated, joined team Pfizer, and I did go jogging today in the park. And I did — this was the mask that I wore with a doctor’s mask under it. And most of the people that I saw that were in the park — the park was packed — I would say like 95% of the people still had masks on.”

The Centers for Disease Control and Prevention (CDC) issued updated guidance for fully vaccinated persons on Tuesday, recommending that they continue to take precautions, such as wearing a “well-fitted mask” while in indoor public settings.
It has always been child abuse
Amen Sis’
sending FAKE messages
America’s leader projects fear and cowardice to other world leaders.
TX casedemic plummets still
NIH science proves masking is unhealthy and not protective against any viru. Why are we still complying?
TEXAS CASEDEMIC DECLINES STILL
NOT AUTHORIZED TO RESTRICT ANYONE!
- STOP OBEYING AMERICA!
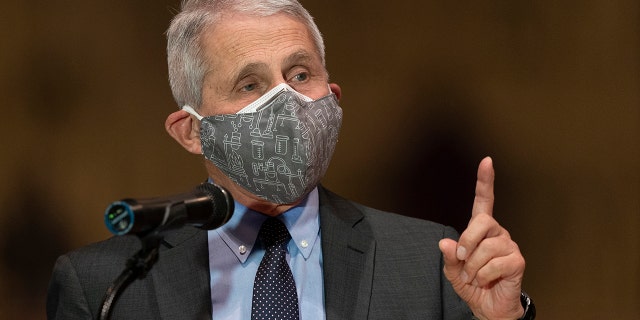
“I don’t enjoy those kind of confrontations, but it was very very clear that he was talking about liberties that were being restricted,” Fauci said. “This has nothing to do with liberties, Dana.
“We’re talking about the fact that 560,000 people have died,” Fauci continued. “We’re talking about 60-70,000 new infections per day. That’s the issue, this is a public health issue, it’s not a civil liberties issue.”
Fauci’s comments come after a Thursday spat between himself and Rep. Jordan. Jordan had asked Fauci when pandemic-related restrictions, rules, and guidelines could be lifted and life could return to normal.
LIBERAL IDIOTS WAKING UP, EVEN
- STOP WEARING FACE DIAPERS OUTDOORS YOU IDIOTS!
- – But still ignore the GOVERNMENT PROVEN SCIENCE they dont work indoors either!
https://thepostmillennial.com/liberal-leaning-slate-tells-readers-stop-wearing-masks-outdoors
– GOVERNMENT ADMISSION MASKING IS A HOAX –
US National Library of Medicine
National Institutes of Health
Facemasks in the COVID-19 era: A health hypothesis
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7680614/
Baruch Vainshelboim⁎Author informationArticle notesCopyright and License informationDisclaimerGo to:
Abstract
Many countries across the globe utilized medical and non-medical facemasks as non-pharmaceutical intervention for reducing the transmission and infectivity of coronavirus disease-2019 (COVID-19). Although, scientific evidence supporting facemasks’ efficacy is lacking, adverse physiological, psychological and health effects are established. Is has been hypothesized that facemasks have compromised safety and efficacy profile and should be avoided from use. The current article comprehensively summarizes scientific evidences with respect to wearing facemasks in the COVID-19 era, providing prosper information for public health and decisions making.Keywords: Physiology, Psychology, Health, SARS-CoV-2, Safety, EfficacyGo to:
Introduction
Facemasks are part of non-pharmaceutical interventions providing some breathing barrier to the mouth and nose that have been utilized for reducing the transmission of respiratory pathogens [1]. Facemasks can be medical and non-medical, where two types of the medical masks primarily used by healthcare workers [1], [2]. The first type is National Institute for Occupational Safety and Health (NIOSH)-certified N95 mask, a filtering face-piece respirator, and the second type is a surgical mask [1]. The designed and intended uses of N95 and surgical masks are different in the type of protection they potentially provide. The N95s are typically composed of electret filter media and seal tightly to the face of the wearer, whereas surgical masks are generally loose fitting and may or may not contain electret-filtering media. The N95s are designed to reduce the wearer’s inhalation exposure to infectious and harmful particles from the environment such as during extermination of insects. In contrast, surgical masks are designed to provide a barrier protection against splash, spittle and other body fluids to spray from the wearer (such as surgeon) to the sterile environment (patient during operation) for reducing the risk of contamination [1].
The third type of facemasks are the non-medical cloth or fabric masks. The non-medical facemasks are made from a variety of woven and non-woven materials such as Polypropylene, Cotton, Polyester, Cellulose, Gauze and Silk. Although non-medical cloth or fabric facemasks are neither a medical device nor personal protective equipment, some standards have been developed by the French Standardization Association (AFNOR Group) to define a minimum performance for filtration and breathability capacity [2]. The current article reviews the scientific evidences with respect to safety and efficacy of wearing facemasks, describing the physiological and psychological effects and the potential long-term consequences on health.Go to:
Hypothesis
On January 30, 2020, the World Health Organization (WHO) announced a global public health emergency of severe acute respiratory syndrome-coronavirus-2 (SARS-CoV-2) causing illness of coronavirus disease-2019 (COVID-19) [3]. As of October 1, 2020, worldwide 34,166,633 cases were reported and 1,018,876 have died with virus diagnosis. Interestingly, 99% of the detected cases with SARS-CoV-2 are asymptomatic or have mild condition, which contradicts with the virus name (severe acute respiratory syndrome-coronavirus-2) [4]. Although infection fatality rate (number of death cases divided by number of reported cases) initially seems quite high 0.029 (2.9%) [4], this overestimation related to limited number of COVID-19 tests performed which biases towards higher rates. Given the fact that asymptomatic or minimally symptomatic cases is several times higher than the number of reported cases, the case fatality rate is considerably less than 1% [5]. This was confirmed by the head of National Institute of Allergy and Infectious Diseases from US stating, “the overall clinical consequences of COVID-19 are similar to those of severe seasonal influenza” [5], having a case fatality rate of approximately 0.1% [5], [6], [7], [8]. In addition, data from hospitalized patients with COVID-19 and general public indicate that the majority of deaths were among older and chronically ill individuals, supporting the possibility that the virus may exacerbates existing conditions but rarely causes death by itself [9], [10]. SARS-CoV-2 primarily affects respiratory system and can cause complications such as acute respiratory distress syndrome (ARDS), respiratory failure and death [3], [9]. It is not clear however, what the scientific and clinical basis for wearing facemasks as protective strategy, given the fact that facemasks restrict breathing, causing hypoxemia and hypercapnia and increase the risk for respiratory complications, self-contamination and exacerbation of existing chronic conditions [2], [11], [12], [13], [14].
Of note, hyperoxia or oxygen supplementation (breathing air with high partial O2 pressures that above the sea levels) has been well established as therapeutic and curative practice for variety acute and chronic conditions including respiratory complications [11], [15]. It fact, the current standard of care practice for treating hospitalized patients with COVID-19 is breathing 100% oxygen [16], [17], [18]. Although several countries mandated wearing facemask in health care settings and public areas, scientific evidences are lacking supporting their efficacy for reducing morbidity or mortality associated with infectious or viral diseases [2], [14], [19]. Therefore, it has been hypothesized: 1) the practice of wearing facemasks has compromised safety and efficacy profile, 2) Both medical and non-medical facemasks are ineffective to reduce human-to-human transmission and infectivity of SARS-CoV-2 and COVID-19, 3) Wearing facemasks has adverse physiological and psychological effects, 4) Long-term consequences of wearing facemasks on health are detrimental.Go to:
Evolution of hypothesis
Breathing Physiology
Breathing is one of the most important physiological functions to sustain life and health. Human body requires a continuous and adequate oxygen (O2) supply to all organs and cells for normal function and survival. Breathing is also an essential process for removing metabolic byproducts [carbon dioxide (CO2)] occurring during cell respiration [12], [13]. It is well established that acute significant deficit in O2 (hypoxemia) and increased levels of CO2 (hypercapnia) even for few minutes can be severely harmful and lethal, while chronic hypoxemia and hypercapnia cause health deterioration, exacerbation of existing conditions, morbidity and ultimately mortality [11], [20], [21], [22]. Emergency medicine demonstrates that 5–6 min of severe hypoxemia during cardiac arrest will cause brain death with extremely poor survival rates [20], [21], [22], [23]. On the other hand, chronic mild or moderate hypoxemia and hypercapnia such as from wearing facemasks resulting in shifting to higher contribution of anaerobic energy metabolism, decrease in pH levels and increase in cells and blood acidity, toxicity, oxidative stress, chronic inflammation, immunosuppression and health deterioration [24], [11], [12], [13].
Efficacy of facemasks
The physical properties of medical and non-medical facemasks suggest that facemasks are ineffective to block viral particles due to their difference in scales [16], [17], [25]. According to the current knowledge, the virus SARS-CoV-2 has a diameter of 60 nm to 140 nm [nanometers (billionth of a meter)] [16], [17], while medical and non-medical facemasks’ thread diameter ranges from 55 µm to 440 µm [micrometers (one millionth of a meter), which is more than 1000 times larger [25]. Due to the difference in sizes between SARS-CoV-2 diameter and facemasks thread diameter (the virus is 1000 times smaller), SARS-CoV-2 can easily pass through any facemask [25]. In addition, the efficiency filtration rate of facemasks is poor, ranging from 0.7% in non-surgical, cotton-gauze woven mask to 26% in cotton sweeter material [2]. With respect to surgical and N95 medical facemasks, the efficiency filtration rate falls to 15% and 58%, respectively when even small gap between the mask and the face exists [25].
Clinical scientific evidence challenges further the efficacy of facemasks to block human-to-human transmission or infectivity. A randomized controlled trial (RCT) of 246 participants [123 (50%) symptomatic)] who were allocated to either wearing or not wearing surgical facemask, assessing viruses transmission including coronavirus [26]. The results of this study showed that among symptomatic individuals (those with fever, cough, sore throat, runny nose ect…) there was no difference between wearing and not wearing facemask for coronavirus droplets transmission of particles of >5 µm. Among asymptomatic individuals, there was no droplets or aerosols coronavirus detected from any participant with or without the mask, suggesting that asymptomatic individuals do not transmit or infect other people [26]. This was further supported by a study on infectivity where 445 asymptomatic individuals were exposed to asymptomatic SARS-CoV-2 carrier (been positive for SARS-CoV-2) using close contact (shared quarantine space) for a median of 4 to 5 days. The study found that none of the 445 individuals was infected with SARS-CoV-2 confirmed by real-time reverse transcription polymerase [27].
A meta-analysis among health care workers found that compared to no masks, surgical mask and N95 respirators were not effective against transmission of viral infections or influenza-like illness based on six RCTs [28]. Using separate analysis of 23 observational studies, this meta-analysis found no protective effect of medical mask or N95 respirators against SARS virus [28]. A recent systematic review of 39 studies including 33,867 participants in community settings (self-report illness), found no difference between N95 respirators versus surgical masks and surgical mask versus no masks in the risk for developing influenza or influenza-like illness, suggesting their ineffectiveness of blocking viral transmissions in community settings [29].
Another meta-analysis of 44 non-RCT studies (n = 25,697 participants) examining the potential risk reduction of facemasks against SARS, middle east respiratory syndrome (MERS) and COVID-19 transmissions [30]. The meta-analysis included four specific studies on COVID-19 transmission (5,929 participants, primarily health-care workers used N95 masks). Although the overall findings showed reduced risk of virus transmission with facemasks, the analysis had severe limitations to draw conclusions. One of the four COVID-19 studies had zero infected cases in both arms, and was excluded from meta-analytic calculation. Other two COVID-19 studies had unadjusted models, and were also excluded from the overall analysis. The meta-analytic results were based on only one COVID-19, one MERS and 8 SARS studies, resulting in high selection bias of the studies and contamination of the results between different viruses. Based on four COVID-19 studies, the meta-analysis failed to demonstrate risk reduction of facemasks for COVID-19 transmission, where the authors reported that the results of meta-analysis have low certainty and are inconclusive [30].
In early publication the WHO stated that “facemasks are not required, as no evidence is available on its usefulness to protect non-sick persons” [14]. In the same publication, the WHO declared that “cloth (e.g. cotton or gauze) masks are not recommended under any circumstance” [14]. Conversely, in later publication the WHO stated that the usage of fabric-made facemasks (Polypropylene, Cotton, Polyester, Cellulose, Gauze and Silk) is a general community practice for “preventing the infected wearer transmitting the virus to others and/or to offer protection to the healthy wearer against infection (prevention)” [2]. The same publication further conflicted itself by stating that due to the lower filtration, breathability and overall performance of fabric facemasks, the usage of woven fabric mask such as cloth, and/or non-woven fabrics, should only be considered for infected persons and not for prevention practice in asymptomatic individuals [2]. The Central for Disease Control and Prevention (CDC) made similar recommendation, stating that only symptomatic persons should consider wearing facemask, while for asymptomatic individuals this practice is not recommended [31]. Consistent with the CDC, clinical scientists from Departments of Infectious Diseases and Microbiology in Australia counsel against facemasks usage for health-care workers, arguing that there is no justification for such practice while normal caring relationship between patients and medical staff could be compromised [32]. Moreover, the WHO repeatedly announced that “at present, there is no direct evidence (from studies on COVID-19) on the effectiveness face masking of healthy people in the community to prevent infection of respiratory viruses, including COVID-19”[2]. Despite these controversies, the potential harms and risks of wearing facemasks were clearly acknowledged. These including self-contamination due to hand practice or non-replaced when the mask is wet, soiled or damaged, development of facial skin lesions, irritant dermatitis or worsening acne and psychological discomfort. Vulnerable populations such as people with mental health disorders, developmental disabilities, hearing problems, those living in hot and humid environments, children and patients with respiratory conditions are at significant health risk for complications and harm [2].
Physiological effects of wearing facemasks
Wearing facemask mechanically restricts breathing by increasing the resistance of air movement during both inhalation and exhalation process [12], [13]. Although, intermittent (several times a week) and repetitive (10–15 breaths for 2–4 sets) increase in respiration resistance may be adaptive for strengthening respiratory muscles [33], [34], prolonged and continues effect of wearing facemask is maladaptive and could be detrimental for health [11], [12], [13]. In normal conditions at the sea level, air contains 20.93% O2 and 0.03% CO2, providing partial pressures of 100 mmHg and 40 mmHg for these gases in the arterial blood, respectively. These gas concentrations significantly altered when breathing occurs through facemask. A trapped air remaining between the mouth, nose and the facemask is rebreathed repeatedly in and out of the body, containing low O2 and high CO2 concentrations, causing hypoxemia and hypercapnia [35], [36], [11], [12], [13]. Severe hypoxemia may also provoke cardiopulmonary and neurological complications and is considered an important clinical sign in cardiopulmonary medicine [37], [38], [39], [40], [41], [42]. Low oxygen content in the arterial blood can cause myocardial ischemia, serious arrhythmias, right or left ventricular dysfunction, dizziness, hypotension, syncope and pulmonary hypertension [43]. Chronic low-grade hypoxemia and hypercapnia as result of using facemask can cause exacerbation of existing cardiopulmonary, metabolic, vascular and neurological conditions [37], [38], [39], [40], [41], [42]. Table 1 summarizes the physiological, psychological effects of wearing facemask and their potential long-term consequences for health.
Table 1
Physiological and Psychological Effects of Wearing Facemask and Their Potential Health Consequences.
| Physiological Effects | Psychological Effect | Health Consequences |
|---|---|---|
| • Hypoxemia• Hypercapnia• Shortness of breath• Increase lactate concentration• Decline in pH levels• Acidosis• Toxicity• Inflammation• Self-contamination• Increase in stress hormones level (adrenaline, noradrenaline and cortisol)• Increased muscle tension• Immunosuppression | • Activation of “fight or flight” stress response• Chronic stress condition• Fear• Mood disturbances• Insomnia• Fatigue• Compromised cognitive performance | • Increased predisposition for viral and infection illnesses• Headaches• Anxiety• Depression• Hypertension• Cardiovascular disease• Cancer• Diabetes• Alzheimer disease• Exacerbation of existing conditions and diseases• Accelerated aging process• Health deterioration• Premature mortality |
In addition to hypoxia and hypercapnia, breathing through facemask residues bacterial and germs components on the inner and outside layer of the facemask. These toxic components are repeatedly rebreathed back into the body, causing self-contamination. Breathing through facemasks also increases temperature and humidity in the space between the mouth and the mask, resulting a release of toxic particles from the mask’s materials [1], [2], [19], [26], [35], [36]. A systematic literature review estimated that aerosol contamination levels of facemasks including 13 to 202,549 different viruses [1]. Rebreathing contaminated air with high bacterial and toxic particle concentrations along with low O2 and high CO2 levels continuously challenge the body homeostasis, causing self-toxicity and immunosuppression [1], [2], [19], [26], [35], [36].
A study on 39 patients with renal disease found that wearing N95 facemask during hemodialysis significantly reduced arterial partial oxygen pressure (from PaO2 101.7 to 92.7 mm Hg), increased respiratory rate (from 16.8 to 18.8 breaths/min), and increased the occurrence of chest discomfort and respiratory distress [35]. Respiratory Protection Standards from Occupational Safety and Health Administration, US Department of Labor states that breathing air with O2 concentration below 19.5% is considered oxygen-deficiency, causing physiological and health adverse effects. These include increased breathing frequency, accelerated heartrate and cognitive impairments related to thinking and coordination [36]. A chronic state of mild hypoxia and hypercapnia has been shown as primarily mechanism for developing cognitive dysfunction based on animal studies and studies in patients with chronic obstructive pulmonary disease [44].
The adverse physiological effects were confirmed in a study of 53 surgeons where surgical facemask were used during a major operation. After 60 min of facemask wearing the oxygen saturation dropped by more than 1% and heart rate increased by approximately five beats/min [45]. Another study among 158 health-care workers using protective personal equipment primarily N95 facemasks reported that 81% (128 workers) developed new headaches during their work shifts as these become mandatory due to COVID-19 outbreak. For those who used the N95 facemask greater than 4 h per day, the likelihood for developing a headache during the work shift was approximately four times higher [Odds ratio = 3.91, 95% CI (1.35–11.31) p = 0.012], while 82.2% of the N95 wearers developed the headache already within ≤10 to 50 min [46].
With respect to cloth facemask, a RCT using four weeks follow up compared the effect of cloth facemask to medical masks and to no masks on the incidence of clinical respiratory illness, influenza-like illness and laboratory-confirmed respiratory virus infections among 1607 participants from 14 hospitals [19]. The results showed that there were no difference between wearing cloth masks, medical masks and no masks for incidence of clinical respiratory illness and laboratory-confirmed respiratory virus infections. However, a large harmful effect with more than 13 times higher risk [Relative Risk = 13.25 95% CI (1.74 to 100.97) was observed for influenza-like illness among those who were wearing cloth masks [19]. The study concluded that cloth masks have significant health and safety issues including moisture retention, reuse, poor filtration and increased risk for infection, providing recommendation against the use of cloth masks [19].
Psychological effects of wearing facemasks
Psychologically, wearing facemask fundamentally has negative effects on the wearer and the nearby person. Basic human-to-human connectivity through face expression is compromised and self-identity is somewhat eliminated [47], [48], [49]. These dehumanizing movements partially delete the uniqueness and individuality of person who wearing the facemask as well as the connected person [49]. Social connections and relationships are basic human needs, which innately inherited in all people, whereas reduced human-to-human connections are associated with poor mental and physical health [50], [51]. Despite escalation in technology and globalization that would presumably foster social connections, scientific findings show that people are becoming increasingly more socially isolated, and the prevalence of loneliness is increasing in last few decades [50], [52]. Poor social connections are closely related to isolation and loneliness, considered significant health related risk factors [50], [51], [52], [53].
A meta-analysis of 91 studies of about 400,000 people showed a 13% increased morality risk among people with low compare to high contact frequency [53]. Another meta-analysis of 148 prospective studies (308,849 participants) found that poor social relationships was associated with 50% increased mortality risk. People who were socially isolated or fell lonely had 45% and 40% increased mortality risk, respectively. These findings were consistent across ages, sex, initial health status, cause of death and follow-up periods [52]. Importantly, the increased risk for mortality was found comparable to smoking and exceeding well-established risk factors such as obesity and physical inactivity [52]. An umbrella review of 40 systematic reviews including 10 meta-analyses demonstrated that compromised social relationships were associated with increased risk of all-cause mortality, depression, anxiety suicide, cancer and overall physical illness [51].
As described earlier, wearing facemasks causing hypoxic and hypercapnic state that constantly challenges the normal homeostasis, and activates “fight or flight” stress response, an important survival mechanism in the human body [11], [12], [13]. The acute stress response includes activation of nervous, endocrine, cardiovascular, and the immune systems [47], [54], [55], [56]. These include activation of the limbic part of the brain, release stress hormones (adrenalin, neuro-adrenalin and cortisol), changes in blood flow distribution (vasodilation of peripheral blood vessels and vasoconstriction of visceral blood vessels) and activation of the immune system response (secretion of macrophages and natural killer cells) [47], [48]. Encountering people who wearing facemasks activates innate stress-fear emotion, which is fundamental to all humans in danger or life threating situations, such as death or unknown, unpredictable outcome. While acute stress response (seconds to minutes) is adaptive reaction to challenges and part of the survival mechanism, chronic and prolonged state of stress-fear is maladaptive and has detrimental effects on physical and mental health. The repeatedly or continuously activated stress-fear response causes the body to operate on survival mode, having sustain increase in blood pressure, pro-inflammatory state and immunosuppression [47], [48].
Long-Term health consequences of wearing facemasks
Long-term practice of wearing facemasks has strong potential for devastating health consequences. Prolonged hypoxic-hypercapnic state compromises normal physiological and psychological balance, deteriorating health and promotes the developing and progression of existing chronic diseases [23], [38], [39], [43], [47], [48], [57], [11], [12], [13]. For instance, ischemic heart disease caused by hypoxic damage to the myocardium is the most common form of cardiovascular disease and is a number one cause of death worldwide (44% of all non-communicable diseases) with 17.9 million deaths occurred in 2016 [57]. Hypoxia also playing an important role in cancer burden [58]. Cellular hypoxia has strong mechanistic feature in promoting cancer initiation, progression, metastasis, predicting clinical outcomes and usually presents a poorer survival in patients with cancer. Most solid tumors present some degree of hypoxia, which is independent predictor of more aggressive disease, resistance to cancer therapies and poorer clinical outcomes [59], [60]. Worth note, cancer is one of the leading causes of death worldwide, with an estimate of more than 18 million new diagnosed cases and 9.6 million cancer-related deaths occurred in 2018 [61].
With respect to mental health, global estimates showing that COVID-19 will cause a catastrophe due to collateral psychological damage such as quarantine, lockdowns, unemployment, economic collapse, social isolation, violence and suicides [62], [63], [64]. Chronic stress along with hypoxic and hypercapnic conditions knocks the body out of balance, and can cause headaches, fatigue, stomach issues, muscle tension, mood disturbances, insomnia and accelerated aging [47], [48], [65], [66], [67]. This state suppressing the immune system to protect the body from viruses and bacteria, decreasing cognitive function, promoting the developing and exacerbating the major health issues including hypertension, cardiovascular disease, diabetes, cancer, Alzheimer disease, rising anxiety and depression states, causes social isolation and loneliness and increasing the risk for prematurely mortality [47], [48], [51], [56], [66].Go to:
Conclusion
The existing scientific evidences challenge the safety and efficacy of wearing facemask as preventive intervention for COVID-19. The data suggest that both medical and non-medical facemasks are ineffective to block human-to-human transmission of viral and infectious disease such SARS-CoV-2 and COVID-19, supporting against the usage of facemasks. Wearing facemasks has been demonstrated to have substantial adverse physiological and psychological effects. These include hypoxia, hypercapnia, shortness of breath, increased acidity and toxicity, activation of fear and stress response, rise in stress hormones, immunosuppression, fatigue, headaches, decline in cognitive performance, predisposition for viral and infectious illnesses, chronic stress, anxiety and depression. Long-term consequences of wearing facemask can cause health deterioration, developing and progression of chronic diseases and premature death. Governments, policy makers and health organizations should utilize prosper and scientific evidence-based approach with respect to wearing facemasks, when the latter is considered as preventive intervention for public health.Go to:
CRediT authorship contribution statement
Baruch Vainshelboim: Conceptualization, Data curation, Writing – original draft.Go to:
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.Go to:
References
1. Fisher E.M., Noti J.D., Lindsley W.G., Blachere F.M., Shaffer R.E. Validation and application of models to predict facemask influenza contamination in healthcare settings. Risk Anal. 2014;34:1423–1434. [PMC free article] [PubMed] [Google Scholar]2. World Health Organization. Advice on the use of masks in the context of COVID-19. Geneva, Switzerland; 2020.3. Sohrabi C., Alsafi Z., O’Neill N., Khan M., Kerwan A., Al-Jabir A. World Health Organization declares global emergency: A review of the 2019 novel coronavirus (COVID-19) Int J Surg. 2020;76:71–76. [PMC free article] [PubMed] [Google Scholar]4. Worldometer. COVID-19 CORONAVIRUS PANDEMIC. 2020.5. Fauci A.S., Lane H.C., Redfield R.R. Covid-19 – Navigating the Uncharted. N Engl J Med. 2020;382:1268–1269. [PMC free article] [PubMed] [Google Scholar]6. Shrestha S.S., Swerdlow D.L., Borse R.H., Prabhu V.S., Finelli L., Atkins C.Y. Estimating the burden of 2009 pandemic influenza A (H1N1) in the United States (April 2009-April 2010) Clin Infect Dis. 2011;52(Suppl 1):S75–S82. [PubMed] [Google Scholar]7. Thompson W.W., Weintraub E., Dhankhar P., Cheng P.Y., Brammer L., Meltzer M.I. Estimates of US influenza-associated deaths made using four different methods. Influenza Other Respir Viruses. 2009;3:37–49. [PMC free article] [PubMed] [Google Scholar]8. Centers for Disease, C., Prevention. Estimates of deaths associated with seasonal influenza — United States, 1976-2007. MMWR Morb Mortal Wkly Rep. 2010,59:1057-62. [PubMed]9. Richardson S., Hirsch J.S., Narasimhan M., Crawford J.M., McGinn T., Davidson K.W. Presenting Characteristics, Comorbidities, and Outcomes Among 5700 Patients Hospitalized With COVID-19 in the New York City Area. JAMA. 2020 [PMC free article] [PubMed] [Google Scholar]10. Ioannidis J.P.A., Axfors C., Contopoulos-Ioannidis D.G. Population-level COVID-19 mortality risk for non-elderly individuals overall and for non-elderly individuals without underlying diseases in pandemic epicenters. Environ Res. 2020;188 [PMC free article] [PubMed] [Google Scholar]11. American College of Sports Medicine . Sixth ed. Lippincott Wiliams & Wilkins; Baltimore: 2010. ACSM’s Resource Manual for Guidelines for Exercise Testing and Priscription. [Google Scholar]12. Farrell P.A., Joyner M.J., Caiozzo V.J. second edition. Lippncott Williams & Wilkins; Baltimore: 2012. ACSM’s Advanced Exercise Physiology. [Google Scholar]13. Kenney W.L., Wilmore J.H., Costill D.L. 5th ed. Human Kinetics; Champaign, IL: 2012. Physiology of sport and exercise. [Google Scholar]14. World Health Organization. Advice on the use of masks in the community, during home care and in health care settings in the context of the novel coronavirus (2019-nCoV) outbreak. Geneva, Switzerland; 2020.15. Sperlich B., Zinner C., Hauser A., Holmberg H.C., Wegrzyk J. The Impact of Hyperoxia on Human Performance and Recovery. Sports Med. 2017;47:429–438. [PubMed] [Google Scholar]16. Wiersinga W.J., Rhodes A., Cheng A.C., Peacock S.J., Prescott H.C. Pathophysiology, Transmission, Diagnosis, and Treatment of Coronavirus Disease 2019 (COVID-19): A Review. JAMA. 2020 [PubMed] [Google Scholar]17. Zhu N., Zhang D., Wang W., Li X., Yang B., Song J. A Novel Coronavirus from Patients with Pneumonia in China, 2019. N Engl J Med. 2020;382:727–733. [PMC free article] [PubMed] [Google Scholar]18. Poston J.T., Patel B.K., Davis A.M. Management of Critically Ill Adults With COVID-19. JAMA. 2020 [PubMed] [Google Scholar]19. MacIntyre C.R., Seale H., Dung T.C., Hien N.T., Nga P.T., Chughtai A.A. A cluster randomised trial of cloth masks compared with medical masks in healthcare workers. BMJ open. 2015;5 [PMC free article] [PubMed] [Google Scholar]20. Patil K.D., Halperin H.R., Becker L.B. Cardiac arrest: resuscitation and reperfusion. Circ Res. 2015;116:2041–2049. [PMC free article] [PubMed] [Google Scholar]21. Hazinski M.F., Nolan J.P., Billi J.E., Bottiger B.W., Bossaert L., de Caen A.R. Part 1: Executive summary: 2010 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations. Circulation. 2010;122:S250–S275. [PubMed] [Google Scholar]22. Kleinman M.E., Goldberger Z.D., Rea T., Swor R.A., Bobrow B.J., Brennan E.E. American Heart Association Focused Update on Adult Basic Life Support and Cardiopulmonary Resuscitation Quality: An Update to the American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2018;137:e7–e13. [PubMed] [Google Scholar]23. Lurie K.G., Nemergut E.C., Yannopoulos D., Sweeney M. The Physiology of Cardiopulmonary Resuscitation. Anesth Analg. 2016;122:767–783. [PubMed] [Google Scholar]24. Chandrasekaran B., Fernandes S. “Exercise with facemask; Are we handling a devil’s sword?” – A physiological hypothesis. Med Hypotheses. 2020;144 [PMC free article] [PubMed] [Google Scholar]25. Konda A., Prakash A., Moss G.A., Schmoldt M., Grant G.D., Guha S. Aerosol Filtration Efficiency of Common Fabrics Used in Respiratory Cloth Masks. ACS Nano. 2020;14:6339–6347. [PMC free article] [PubMed] [Google Scholar]26. Leung N.H.L., Chu D.K.W., Shiu E.Y.C., Chan K.H., McDevitt J.J., Hau B.J.P. Respiratory virus shedding in exhaled breath and efficacy of face masks. Nat Med. 2020;26:676–680. [PubMed] [Google Scholar]27. Gao M., Yang L., Chen X., Deng Y., Yang S., Xu H. A study on infectivity of asymptomatic SARS-CoV-2 carriers. Respir Med. 2020;169 [PMC free article] [PubMed] [Google Scholar]28. Smith J.D., MacDougall C.C., Johnstone J., Copes R.A., Schwartz B., Garber G.E. Effectiveness of N95 respirators versus surgical masks in protecting health care workers from acute respiratory infection: a systematic review and meta-analysis. CMAJ. 2016;188:567–574. [PMC free article] [PubMed] [Google Scholar]29. Chou R., Dana T., Jungbauer R., Weeks C., McDonagh M.S. Masks for Prevention of Respiratory Virus Infections, Including SARS-CoV-2, in Health Care and Community Settings: A Living Rapid Review. Ann Intern Med. 2020 [PMC free article] [PubMed] [Google Scholar]30. Chu D.K., Akl E.A., Duda S., Solo K., Yaacoub S., Schunemann H.J. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: a systematic review and meta-analysis. Lancet. 2020;395:1973–1987. [PMC free article] [PubMed] [Google Scholar]31. Center for Disease Control and Prevention. Implementation of Mitigation Strategies for Communities with Local COVID-19 Transmission. Atlanta, Georgia; 2020.32. Isaacs D., Britton P., Howard-Jones A., Kesson A., Khatami A., Marais B. Do facemasks protect against COVID-19? J Paediatr Child Health. 2020;56:976–977. [PMC free article] [PubMed] [Google Scholar]33. Laveneziana P., Albuquerque A., Aliverti A., Babb T., Barreiro E., Dres M. ERS statement on respiratory muscle testing at rest and during exercise. Eur Respir J. 2019;53 [PubMed] [Google Scholar]34. American Thoracic Society/European Respiratory, S ATS/ERS Statement on respiratory muscle testing. Am J Respir Crit Care Med. 2002;166:518–624. [PubMed] [Google Scholar]35. Kao T.W., Huang K.C., Huang Y.L., Tsai T.J., Hsieh B.S., Wu M.S. The physiological impact of wearing an N95 mask during hemodialysis as a precaution against SARS in patients with end-stage renal disease. J Formos Med Assoc. 2004;103:624–628. [PubMed] [Google Scholar]36. United States Department of Labor. Occupational Safety and Health Administration. Respiratory Protection Standard, 29 CFR 1910.134; 2007.37. ATS/ACCP Statement on cardiopulmonary exercise testing Am J Respir Crit Care Med. 2003;167:211–277. [PubMed] [Google Scholar]38. American College of Sports Medicine . 9th ed. Wolters Kluwer/Lippincott Williams & Wilkins Health; Philadelphia: 2014. ACSM’s guidelines for exercise testing and prescription. [Google Scholar]39. Balady G.J., Arena R., Sietsema K., Myers J., Coke L., Fletcher G.F. Clinician’s Guide to cardiopulmonary exercise testing in adults: a scientific statement from the American Heart Association. Circulation. 2010;122:191–225. [PubMed] [Google Scholar]40. Ferrazza A.M., Martolini D., Valli G., Palange P. Cardiopulmonary exercise testing in the functional and prognostic evaluation of patients with pulmonary diseases. Respiration. 2009;77:3–17. [PubMed] [Google Scholar]41. Fletcher G.F., Ades P.A., Kligfield P., Arena R., Balady G.J., Bittner V.A. Exercise standards for testing and training: a scientific statement from the American Heart Association. Circulation. 2013;128:873–934. [PubMed] [Google Scholar]42. Guazzi M., Adams V., Conraads V., Halle M., Mezzani A., Vanhees L. EACPR/AHA Scientific Statement. Clinical recommendations for cardiopulmonary exercise testing data assessment in specific patient populations. Circulation. 2012;126:2261–2274. [PMC free article] [PubMed] [Google Scholar]43. Naeije R., Dedobbeleer C. Pulmonary hypertension and the right ventricle in hypoxia. Exp Physiol. 2013;98:1247–1256. [PubMed] [Google Scholar]44. Zheng G.Q., Wang Y., Wang X.T. Chronic hypoxia-hypercapnia influences cognitive function: a possible new model of cognitive dysfunction in chronic obstructive pulmonary disease. Med Hypotheses. 2008;71:111–113. [PubMed] [Google Scholar]45. Beder A., Buyukkocak U., Sabuncuoglu H., Keskil Z.A., Keskil S. Preliminary report on surgical mask induced deoxygenation during major surgery. Neurocirugia (Astur) 2008;19:121–126. [PubMed] [Google Scholar]46. Ong J.J.Y., Bharatendu C., Goh Y., Tang J.Z.Y., Sooi K.W.X., Tan Y.L. Headaches Associated With Personal Protective Equipment – A Cross-Sectional Study Among Frontline Healthcare Workers During COVID-19. Headache. 2020;60:864–877. [PubMed] [Google Scholar]47. Schneiderman N., Ironson G., Siegel S.D. Stress and health: psychological, behavioral, and biological determinants. Annu Rev Clin Psychol. 2005;1:607–628. [PMC free article] [PubMed] [Google Scholar]48. Thoits P.A. Stress and health: major findings and policy implications. J Health Soc Behav. 2010;51(Suppl):S41–S53. [PubMed] [Google Scholar]49. Haslam N. Dehumanization: an integrative review. Pers Soc Psychol Rev. 2006;10:252–264. [PubMed] [Google Scholar]50. Cohen S. Social relationships and health. Am Psychol. 2004;59:676–684. [PubMed] [Google Scholar]51. Leigh-Hunt N., Bagguley D., Bash K., Turner V., Turnbull S., Valtorta N. An overview of systematic reviews on the public health consequences of social isolation and loneliness. Public Health. 2017;152:157–171. [PubMed] [Google Scholar]52. Holt-Lunstad J., Smith T.B., Layton J.B. Social relationships and mortality risk: a meta-analytic review. PLoS Med. 2010;7 [PMC free article] [PubMed] [Google Scholar]53. Shor E., Roelfs D.J. Social contact frequency and all-cause mortality: a meta-analysis and meta-regression. Soc Sci Med. 2015;128:76–86. [PubMed] [Google Scholar]54. McEwen B.S. Protective and damaging effects of stress mediators. N Engl J Med. 1998;338:171–179. [PubMed] [Google Scholar]55. McEwen B.S. Physiology and neurobiology of stress and adaptation: central role of the brain. Physiol Rev. 2007;87:873–904. [PubMed] [Google Scholar]56. Everly G.S., Lating J.M. 4th ed. NY Springer Nature; New York: 2019. A Clinical Guide to the Treatment of the Human Stress Response. [Google Scholar]57. World Health Organization. World health statistics 2018: monitoring health for the SDGs, sustainable development goals Geneva, Switzerland; 2018.58. World Health Organization. World Cancer Report 2014. Lyon; 2014.59. Wiggins J.M., Opoku-Acheampong A.B., Baumfalk D.R., Siemann D.W., Behnke B.J. Exercise and the Tumor Microenvironment: Potential Therapeutic Implications. Exerc Sport Sci Rev. 2018;46:56–64. [PubMed] [Google Scholar]60. Ashcraft K.A., Warner A.B., Jones L.W., Dewhirst M.W. Exercise as Adjunct Therapy in Cancer. Semin Radiat Oncol. 2019;29:16–24. [PMC free article] [PubMed] [Google Scholar]61. Bray F., Ferlay J., Soerjomataram I., Siegel R.L., Torre L.A., Jemal A. Global Cancer Statistics 2018: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin. 2018 [PubMed] [Google Scholar]62. Brooks S.K., Webster R.K., Smith L.E., Woodland L., Wessely S., Greenberg N. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395:912–920. [PMC free article] [PubMed] [Google Scholar]63. Galea S., Merchant R.M., Lurie N. The Mental Health Consequences of COVID-19 and Physical Distancing: The Need for Prevention and Early Intervention. JAMA Intern Med. 2020;180:817–818. [PubMed] [Google Scholar]64. Izaguirre-Torres D., Siche R. Covid-19 disease will cause a global catastrophe in terms of mental health: A hypothesis. Med Hypotheses. 2020;143 [PMC free article] [PubMed] [Google Scholar]65. Kudielka B.M., Wust S. Human models in acute and chronic stress: assessing determinants of individual hypothalamus-pituitary-adrenal axis activity and reactivity. Stress. 2010;13:1–14. [PubMed] [Google Scholar]66. Morey J.N., Boggero I.A., Scott A.B., Segerstrom S.C. Current Directions in Stress and Human Immune Function. Curr Opin Psychol. 2015;5:13–17. [PMC free article] [PubMed] [Google Scholar]67. Sapolsky R.M., Romero L.M., Munck A.U. How do glucocorticoids influence stress responses? Integrating permissive, suppressive, stimulatory, and preparative actions. Endocr Rev. 2000;21:55–89. [PubMed] [Google Scholar]
H O A X
FAUCI IS A GOT DAM LIAR
ADMISSION: MEDIAs virus DEATH TICKER side PANES PROMOTED VIRUS HYPE
- NOT THERE FOR ANYTHING OTHER THAN HYPE

MONTANA GOV DENIES VAX PASSPORTS
Montana Gov. Greg Gianforte signed an executive order banning vaccine passports on Tuesday, prohibiting state agencies and businesses from requiring people to show proof of vaccination before providing their services.
TX GOV ABBOTT SHOULD TAKE NOTES!
FAUCI=Criminal
Infectious disease expert Dr. Steven Hatfill confirms hydroxychloroquine-based medicine’s efficacy against the CCP (Communist Party of China) Virus. He has condemned Dr. Anthony Fauci and others’ intentional interference against the drug’s use, despite its proven effectiveness.
“It’s pretty clear that Dr. Fauci, Dr. Woodcock and Dr. [Rick] Bright are responsible for hundreds of thousands of deaths in the United States for giving this drug a bad name,” Dr. Hatfill said on Steve Bannon’s War Room program on April 13.
THIS TIME IT WONT GET DELETED
CASEDEMIC decline
FAUCI = LIAR
FIRE THIS A HOLE AMERICA!
Stop obeying the unlawful chinavirus hoax mandates!
Texas case-demic continues to decline
As Breitbart News has continued to note, CDC data separates New York City’s data from the remainder of the state. Even so, New York, excluding the city, has reported 239.9 cases per 100,000 in the last seven days, or 26,525 cases.
New York City specifically reported 289.4 cases per 100,000, or 24,303 in the same time frame. Combined, the Empire State has reported 50,828 cases in the last seven days.
Texas, which lifted coronavirus-related restrictions last month, including the statewide mask mandate which had remained in effect since last summer, is also faring far better than those blue states, reporting 64.6 new cases of the virus per 100,000 in the last seven days, or 18,731 cases total.
Teacher Union hypocrites going out and enjoying themselves. Keeping schools closed.

But even as she herself goes out to dinner with other people, Weingarten is working hard as the leader of the country’s second-largest teachers union to keep classrooms closed to American children, citing safety concerns for faculty and staff.
Luther was found to have had her civil rights violated by local court,by TX supremes
Dallas Hair Salon Owner Shelley Luther Victorious as Texas Supreme Court Voids Contempt Order
While she’s cleared this hurdle, Luther and her business continue to be persecuted by the City of Dallas. It’s unclear how this ruling will affect Luther’s still pending legal fight with the city.
“We’re grateful for the support we’ve received from individuals across the country, and we ask that you continue to lift us up in prayer.”
Unfortunately, the state of Texas is currently contemplating legislation in House Bill 3 and Senate Bill 6 that would set up business owners with the same liability Luther has been forced to confront in these legal proceedings.
Specifically, these bills force businesses to comply with CDC guidelines that change often and aren’t set by elected officials but nameless faceless bureaucrats. Currently, these guidelines include recommended double masking and mandate mask-wearing by 2-year-olds!
“What happened to me can happen again. Lawmakers need to protect business owners from busy body bureaucrats, not whitewash pandemic power grabs, empowering similar behavior in the future.”
Social distancing is a hoax
NH track coach refuses mask hoax mandate: fired
I’ll come straight to the point,” Keyes wrote. “I will not put kids on the track and tell them to run any races while wearing masks.”
Keyes was responding to recommendations put out by the New Hampshire Interscholastic Athletic Association stating, “It is recommended that athletes wear a face covering during competition in all events.”
“No, the real reason I won’t do it is because it’s senseless, irrational, cowardice b——t and I will not help cover that up,” Keyes’ letter stated. “I will not stand up in front of the kids and lie to them and tell them that these masks are doing anything worthwhile out in an open field with wind blowing and the sun shining.”
“Fire me if you must,” Keyes said in a follow-up message. On Monday, Keyes was terminated.
Speaking to NBC10 Boston, the now-fired track and field coach explained he’s against masks for runners because they restrict the essential act of breathing.
“Masks restrict breathing, there’s no question about it, especially think about running full-speed. The wind is in your face, it’s shoving the mask back into your nose and mouth.”
A student interviewed by CBS Boston said Keyes was one of his favorite coaches, adding masks are untenable for runners, especially in hot weather.
In a farewell message left at the Pembroke Academy website, Keyes explained mask rules will be violated by some coaches and obeyed by others, creating an un-level playing field amongst athletes.
..until they do
White House press secretary Jen Psaki downplayed government support for a vaccine passport system Tuesday, asserting the administration did not support requiring Americans to carry a vaccine credential.
VAX DOES NOT PREVENT INFECTIONS
Nearly 250 people who have been fully vaccinated against COVID-19 have tested positive for the virus, the Michigan Department of Health and Human Services said.
According to MDHHS, 246 people have had a positive test 14 or more days after receiving their second dose of the vaccine as of the end of March. The people who have tested positive have been asymptomatic or have had milder symptoms compared to unvaccinated people
SOUTH DAKOTA – SWEDEN MODEL
Although South Dakota has the eighth highest death rate among US states, its epidemic retreated without any government intervention. (And no new restrictions were introduced in March or the first week of April.)
South Dakota currently has the lowest unemployment rate out of all 50 states – at just 2.9%.
Virus Surface transmission was a hoax; LIES to make sure Trump didn’t win the presidency again.
The Centers for Disease Control and Prevention said Monday there is no significant risk of catching the coronavirus from a surface or object.
The CDC clarified its position in a guidance update that said people generally contract COVID-19 through direct contact with a sick person or from airborne transmission.
https://nypost.com/2021/04/05/low-risk-of-catching-covid-from-surfaces-new-cdc-guidelines/
TX Governor Abbott BANS vaccine passports? ( NOPE HE DIDN’T )
Texans shouldn’t be required to show proof of vaccination & reveal private health information just to go about their daily lives.
I issued an Executive Order that prohibits government-mandated vaccine passports in Texas.
Don’t tread on our personal freedoms. https://pic.twitter.com/weTbz4FKyH
Abbott’s order merely prevents government-mandated vaccine passports
with the vast majority of private businesses remaining unaffected.
Only private businesses that received government money are prevented from requiring vaccine passports, meaning it would be almost impossible for the average citizen to know if a business that requires a vaccine passport is in compliance with the executive order or not. Nursing homes and elder care facilities are exempt regardless of their public or private status.
I’m not really quite sure. It could be they’re doing things outdoors.”
Texas is experiencing a ( MASSIVE ) decline in COVID-19 cases
This is not ‘normal’

Needs no caption

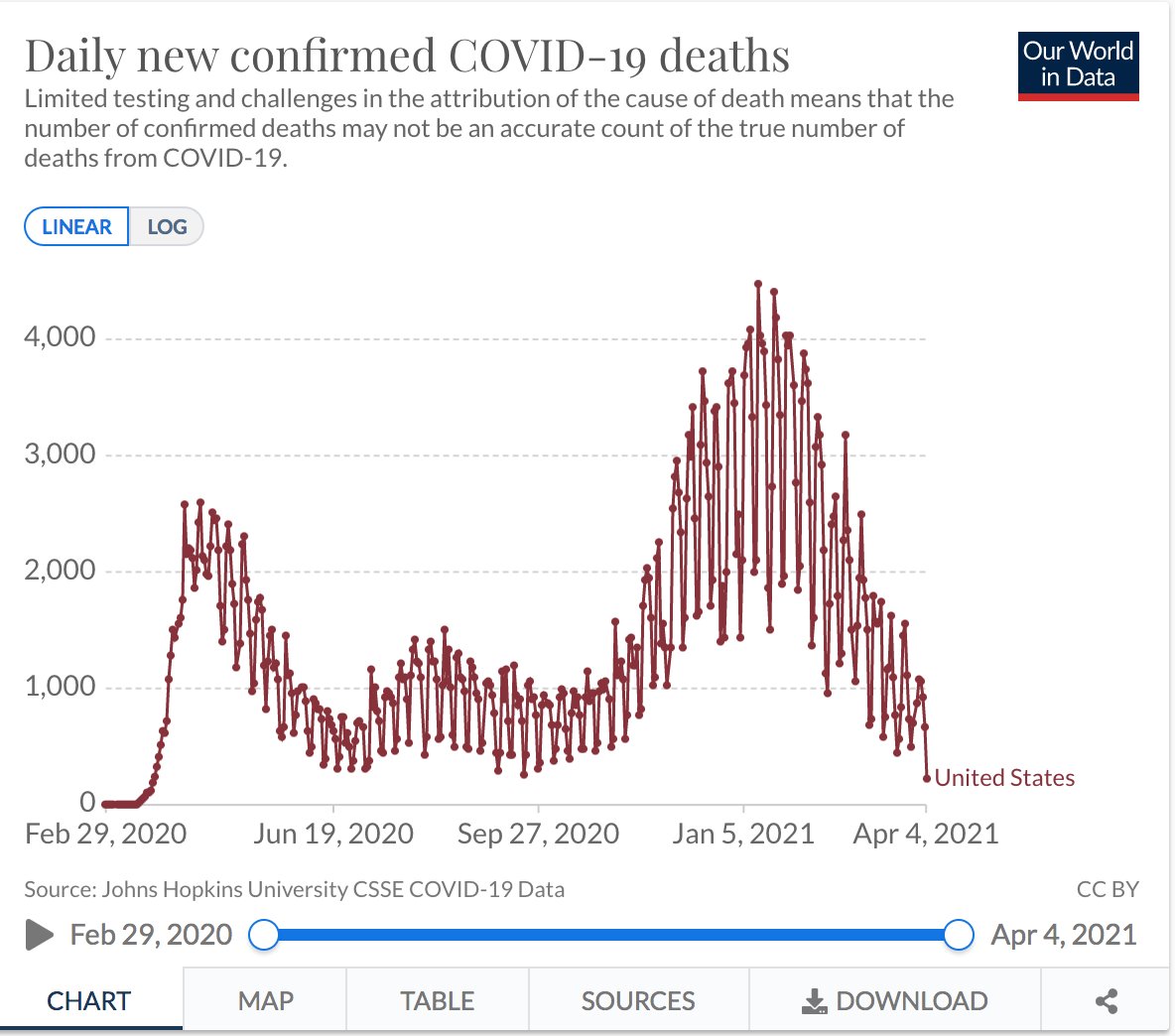
The number of COVID-19 deaths per day in the U.S. dropped to its lowest point in more than a year on Sunday, with the country documenting 222 fatalities.
MASKing HOAX EXPOSED DAILY
Texas, which lifted its mask mandate last month to the dismay of many, reported 76.5 cases per 100,000, or 22,194 in the last seven days.
April 2 CDC data, which separates New York data from the New York City data, the Empire State, minus the city, reported 256.7 cases of the virus per 100,000 in the last seven days, or 28,375 cases total.
New York City reported 353.6 cases per 100,000, or 29,695 cases.
Combined, that is 58,070 cases across the state in the last week.
Michigan has reported 411.1 cases per 100,000, or 41,056 total in the same time frame.
Social distancing is a hoax
Mask hoax lawsuits begin!
https://abc13.com/education/5-parents-suing-katy-isd-over-districts-mask-mandate/10470293/
CNN COMMUNIST & baby killing advocate chief WANTS YOU LOCKED DOWN IF YOU DONT OBEY/VAX
“Because otherwise, if everything is reopened, then what’s the carrot going to be? How are we going to incentivize people to actually get the vaccine? So that’s why I think the CDC and the Biden administration needs to come out a lot bolder and say, ‘If you are vaccinated, you can do all these things. Here are all these freedoms that you have.’ Because otherwise, people are going to go out and enjoy these freedoms anyway.'”
Unconstitutional
The Wisconsin Supreme Court has struck down a mask mandate put in place by Democrat Gov. Tony Evers.
In a crucial 4-3 ruling, the state’s Supreme Court ruled that Evers mandate exceeded his authority.
CDC doomer does backflip from previous statement
On Monday’s broadcast of MSNBC’s “Rachel Maddow Show,” CDC Director Dr. Rochelle Walensky stated that CDC data released earlier in the day “suggests that vaccinated people do not carry the virus, don’t get sick, and that it’s not just in the clinical trials, but it’s also in real-world data.”
AR WANTS RIGHT “MESSAGE” SENT in RESTRICTING BASIC AMERICAN CIVIL RIGHTS
- RECALL THESE PEOPLE AR!
LITTLE ROCK, Ark. (AP) — Arkansas lawmakers have rejected an effort to end the emergency declared in the state because of the coronavirus pandemic.
The Arkansas Legislative Council made the move on Monday, effectively voting to allow the governor to keep his emergency powers to curb the virus’ spread for another two months. Gov. Asa Hutchinson urged lawmakers to allow him to continue the emergency declaration, saying ending it would send the wrong message.
COMMUNISTS PUSHING VAX “PASSPORTS” FOR DOMESTIC MOVEMENT
There is evidence vaccine passports could motivate skeptical Americans to get shots. Several vaccine-hesitant participants at a recent focus group of Trump voters led by pollster Frank Luntz suggested their desire to see family, go on vacation and resume other aspects of daily life outpaced fear of the shots, particularly if travel companies and others moved to require proof of vaccination.
.@naomirwolf sounds the alarm on the push for 'vaccine passports': "I am not overstating this, I can't say it forcefully enough, this is literally the end of human liberty in the West if this plan unfolds…"#NextRevFNC pic.twitter.com/rmAC3YKKP4
— The Next Revolution (@NextRevFNC) March 29, 2021
Don’t be a got dam mask karen

6 feet is a hoax
Gottlieb added that it isn’t clear where the six-feet directive derived from since the CDC has failed to reference specific studies that support that figure. He recommended that President Joe Biden’s administration revisits guidelines and loosens restrictions.
Chinavax papers required in NY for many locations
It’s Official. “Vaccine Passports” Are Required In New York
Children mostly unaffected by chinavirus
(CNSNews.com) – Of the 526,028 deaths in the United States involving COVID-19, as officially reported by the Centers for Disease Control and Prevention, 238 have been in children 17 and younger.
That equals 0.04 percent of all COVID-19 deaths reported in the United States.
The largest number of COVID-19 deaths was among people 85 and older (162,583), according to the CDC. That was followed by 146,310 COVID-19 deaths in people 75 to 84; 115,381 in people 65 to 74; 78,883 in people 50 to 64; 15,134 in people 40 to 49; 5,583 in people 30 to 39; and 1,916 in people 18 to 29.According to the death certificate data reported by the CDC as of March 24, 526,028 people had deaths involving COVID-19. Of those, 238 were 17 or younger.
According to the CDC it can take multiple weeks for death certificates to reach the National Center for Health Statistics.
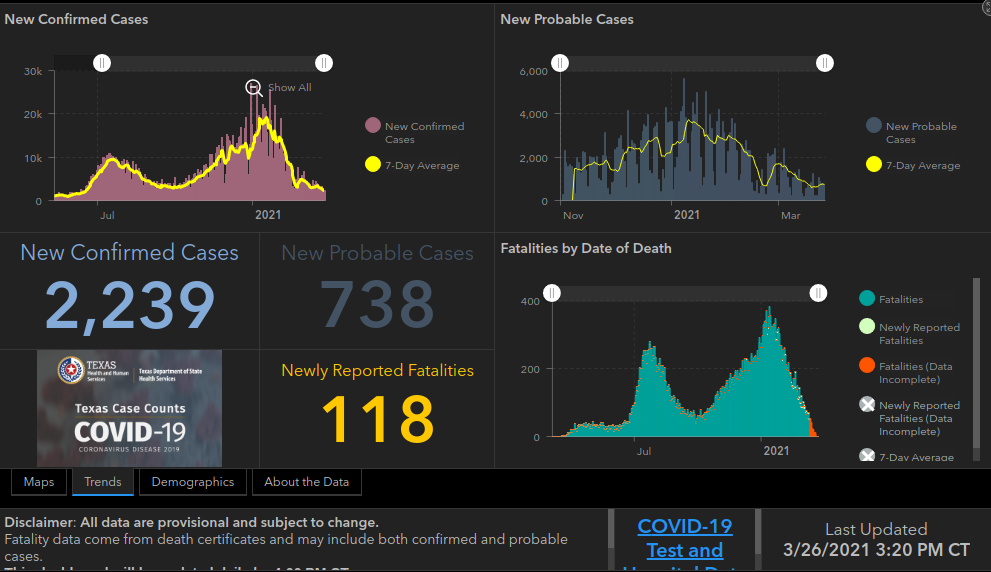
MASKED NY WORSE OFF THAN unmasked FL TX
According to the CDC’s March 26 data, Florida reported 151.8 new cases of the virus per 100,000 in the last seven days, or 32,608 cases in that time period, total. Texas reported just 83 cases per capita, or 24,055 total in the last seven days.
In contrast, New York has reported 225.3 cases per 100,000 in the last seven days, or 24,909 total.
White House press secretary Jen Psaki said, “The entire country has paid the price for political leaders who ignore the science,” and actor Matthews McConaughey even spoke out about his home state.
“I was a little dumbfounded by the decision,” McConaughey said on “CBS This Morning.” “I understand ‘go back to work.’ What I did not understand was ‘pull the mask mandate.’”
California Gov. Gavin Newsom called the move “absolutely reckless,” and Twitter was flooded with hot takes from people who called Abbott’s decision everything from “crazy” to “embarrassing.”
THE SWEDEN / SOUTH DAKOTA SUCCESS
Preliminary data from EU statistics agency Eurostat compiled by Reuters showed Sweden had 7.7% more deaths in 2020 than its average for the preceding four years. Countries that opted for several periods of strict lockdowns, such as Spain and Belgium, had so-called excess mortality of 18.1% and 16.2% respectively.
BOTH of these masks are worthless, stupid, embarrassing and not science.
- DONT COMPLY AMERICA!

AMERICAN IDIOTS IN GOVT ADMIT IT WRECKED ITSELF FOR CHICOM VIRUS WARFARE BY CCP
A former top U.S. health official says he thinks the coronavirus originated in a lab in Wuhan, China, and began spreading as early as September 2019.
Robert Redfield, who led the U.S. Centers for Disease Control and Prevention during the first year of the COVID-19 pandemic, told CNN in a clip aired Friday that he thinks that scenario is more likely than any alternative, including that the virus erupted after transferring from animals to humans or in a live animal market.
FL GOV DESANTIS ADMITS SHUTDOWN WRONG-
Gov. Ron DeSantis (R) regrets locking down the state during the pandemic “for even one day,” Rep. Matt Gaetz (R-FL) said, according to Politico.
Florida Governor Ron DeSantis announced that the Sunshine State won’t have any part in issuing vaccine passports, calling it a “bad idea.”
MASK KAREN FAUCI IS MASKING FOR THEATER
CDC: 3 feet is OK now
This is a lie. Stop obeying America.
Those exposed prior to getting a vax, dont need it.
U.S. administers 105.7 million doses of COVID-19 vaccines: CDC
CDC recommends child-abuse
The new CDC guidance calls for mask-wearing for children aged two and older:
Everyone 2 years and older should wear a mask covering their mouth and nose when around people who do not live in their household, except when eating or sleeping.
3 FEET AND YOU WONT DIE!
The United States’ top pandemic advisor said Sunday that authorities were considering cutting social distancing rules to three feet (one meter), a move that would change a key tenet of the global fight against Covid-19.
MI GOV WHITMER PROSECUTION FOR MURDERING OLD FOLKS?
Macomb County, Michigan, prosecutor Peter Lucido (R) said Thursday he has received “hundreds” of calls and emails with information that could aid an investigation into coronavirus-related nursing home deaths
“biggest public health mistake we’ve ever made
Bhattacharya also noted that “the lockdown harms are worse than COVID” and that “the harm to people is catastrophic.” His reasoning is that “public health” means a whole lot more than protection from a virus, and that people need many more things in life in order to stay healthy — not only physically but also mentally and emotionally — such as interaction with friends and the ability to earn a living, which lockdowns have prevented.
I stand behind my comment that the lockdowns are the single worst public health mistake in the last 100 years. We will be counting the catastrophic health and psychological harms, imposed on nearly every poor person on the face of the earth, for a generation.
At the same time, they have not served to control the epidemic in the places where they have been most vigorously imposed. In the US, they have — at best — protected the “non-essential” class from COVID, while exposing the essential working class to the disease. The lockdowns are trickle down epidemiology.
https://www.theblaze.com/news/stanford-prof-lockdowns-biggest-public-health-mistake
CHI-COM SUPPORTING WHITEHOUSE OCCUPANT:
- AMERICANS MUST NOT COMPLY -EVER AGAIN
We will issue guidance on what you can and cannot do when fully vaccinated,” Biden said.
“Listen to Dr. Fauci,” Biden said — or else. “If we don’t stay vigilant, and the conditions change, then we may have to reinstate restrictions.”
…so the point of vaxxing is?
On Thursday’s broadcast of CNN’s “AC360,” CDC Director Dr. Rochelle Walensky stated that it’s “too early to project when we can lose our masks.”
NO MEDICAL NECESSITY FOR VACCINE PASSPORTS
Democrat controlled NY school mandating double masking for children!

A middle school in New York is mandating “Double masks” for all students beginning March 15, according to a principal’s message posted to a parents’ group. East Hampton Middle School principal Dr. Charles Soriano said that “Double masking — wearing a disposable, medical procedure mask underneath a cloth mask — will be a school requirement” and “This is not optional.”
TEXAS NOW FREE FROM MASKING HOAX
Texas can now breath freely and are now able to walk in public without the threat of arrest. Texas should replace RINO GOV ABBOTT with a GIRL like SD GOV. NOEM!
- Businesses will now get to decide to follow science, or create a use of force by government against people walking in their store ‘unmasked’.
WELL KNOWN PROBLEM OF NOBODY CAN HEAR CLEARLY, MASKERS TALKING
Tucker Carlson and Alex Berenson discuss how the Federal Aviation Administration (FAA) management's weird obsession with (apparently) forcing air traffic controllers to wear face masks when talking to pilots could lead to devastating consequences. pic.twitter.com/aw0ojYLfA1
— Scott Morefield (@SKMorefield) March 9, 2021
Berenson appeared on Fox News Monday night to talk about the national security issue.
He told host Tucker Carlson that the FAA whistleblower said that people should be aware that requiring air traffic controllers to wear masks is creating a “real risk.”
“Several thousand people have retweeted that and now I’m talking to you about it so hopefully someone at the FAA will pay a little attention to this,” Berenson said.
CLOSING SCHOOL WAS -ALWAYS- CHILD-ABUSE!
Medical experts say that the Centers for Disease Control and Prevention should issue science-based guidance and allow U.S. schools to reopen. The authorities, who include pediatricians, epidemiologists, and infectious disease experts, say the agency’s current school reopening guidance is based on fear, not fact.
Half the schools in America are closed and more are only partially open.
Drs. Tara O. Henderson, Monica Gandhi, Tracy Beth Hoeg, and Daniel Johnson wrote an opinion piece in USA Today saying that keeping schools closed or even partially reopened is “unwarranted, harming children, and has become a human rights issue.”
NEW CHINAVIRUS STRAIN PANIC PORN FAKE NEWS
An American physician said the U.S. is on track to overcome coronavirus and finally reopen. In an interview over the weekend, former FDA chief Dr. Scott Gottlieb asserted a resurgence of COVID-19 is unlikely despite reports of so-called “new strains.”
“There’s probably some crossover between the immunity you get from B.1.1.7 and immunity against those other strains,” he explained. “I don’t think we’re going to see another surge of infection this spring, but we might see a plateauing before we see continued declines again.”
Dr. Gottlieb added, the decline in new COVID infections may slow down in coming weeks, but then it will dramatically reduce by early summer due to ongoing vaccinations. He said COVID strains are mere variations of the same virus, which the human immune system is able to handle.
Double Masked Vaxxed Prez


Chicom Virus executive order criminal-negligence mounts for NY GOV Cuomo
As New York Gov. Andrew Cuomo (D) faces articles of impeachment over covering up COVID-19 deaths in nursing homes and multiple allegations of sexual harassment, there is renewed scrutiny of his administration’s mishandling of the pandemic, including focus on an executive order that required homes for people with developmental disabilities to accept coronavirus patients.
BIDEN IS IN, OPEN NYC SCHOOLS!
New York City will welcome high school students back into classrooms starting on March 22, Mayor Bill de Blasio announced on Monday, a major milestone in the city’s sometimes halting efforts to resume in-person instruction for some of its one million students.
LOCK HER UP !
Macomb County Prosecutor Peter Lucido is contemplating bringing charges against Whitmer for any of the deaths associated with the decision. The problem, however, is HIPAA laws prevent the prosecutor’s office from receiving vital information about a patient’s death. The only way Lucido’s office would receive the information is if a relative lodged a wrongful death complaint with the local police department.
In order for charges to be brought about, family members have to request data and additional information surrounding the person’s death. It’s something Lucido is encouraging family members to do if a loved one died.